What is osteoporosis?
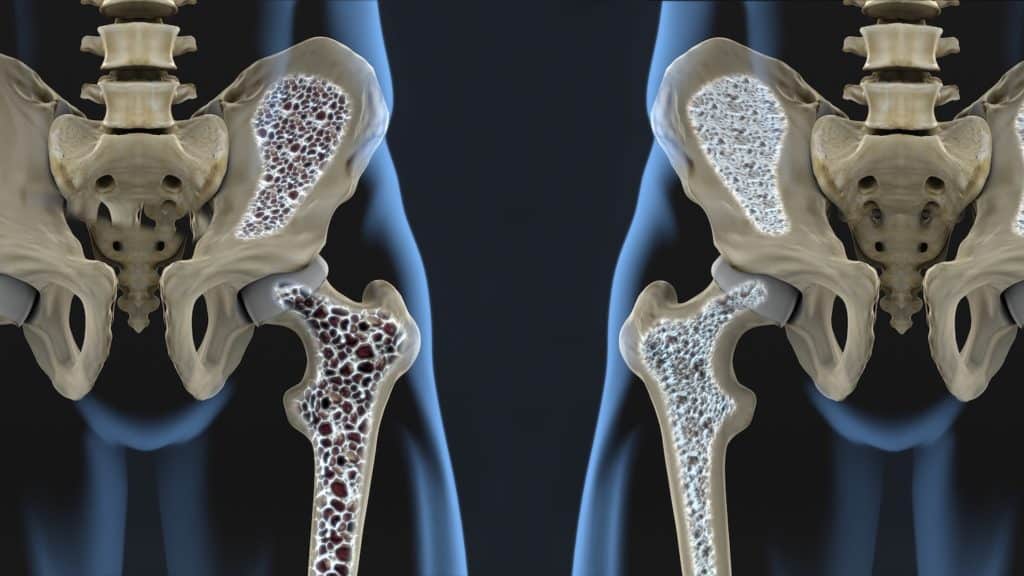
Osteoporosis is a disease that affects your bones. It makes them fragile and more likely to break. Osteoporosis develops slowly over a long time and is usually only diagnosed when a sudden break appears after an injury. The most common injuries among people with osteoporosis are broken wrists, hips, or spinal bones.
Of course, as all bones are affected, breaks in arms, legs or pelvis are possible. If osteoporosis is severe enough, in some instances coughing or sneezing can cause a broken rib.
There is not usually pain associated with osteoporosis until you break a bone, however, broken bones, especially in critical areas like the spine may cause long-term pain.
Before the diagnosis of osteoporosis people may suffer from osteopenia. This is when scans detect that you have lower bone density than average for your age group, but not low enough to class it as osteoporosis.
Osteopenia does not always lead to osteoporosis as there are things you can do to keep your bones healthy and reduce your risk of developing the more serious disease.
Who is at risk of osteoporosis?
Among many doctors, osteoporosis is often known as a silent disease. This is because while almost 3 million people in the UK are estimated to have osteoporosis very few of them know they have it until they break a bone. More than 300,000 fractures are attributed to osteoporosis every year.
Osteoporosis is more common among older people. Around 1 in 3 women and 1 in 5 men over the age of 50 will break or fracture a bone due to osteoporosis (Age UK, 2021).
Causes of osteoporosis
Human bones are at their peak strength in their early adult life until your late 20s. From around 35, you start losing bone gradually. Osteoporosis can affect both men and women. It is more common among older people but there are recorded cases among people of a young age (NHS, 2019).
Women
Unfortunately, women are more at risk of developing osteoporosis due to the hormonal changes that happen at menopause which directly affect bone density.
Oestrogen, the female hormone, is critical for healthy bones. After menopause oestrogen levels drop and this can lead to a higher decrease in bone density.
Females are at even higher risk of developing osteoporosis if they have any of the following:
- Early menopause
- Hysterectomy before the age of 45
- Absent periods for more than 6 months due to over exercising or too much dieting
Men
The cause of osteoporosis among men is not known in many cases. However, there has been a link established between the male hormone testosterone which aids with bone health. Men do continue to produce testosterone even when they are older, so the risk of osteoporosis is increased only among the men who produce lower levels of this hormone
The most known causes of osteoporosis among men are from:
- Certain medications such as steroids
- Consuming too much alcohol
- Hypogonadism
Other risk factors
Some factors that may increase the risk of developing osteoporosis are not gender specific. If you have any disorders of the hormone-producing glands, then you may be at higher risk. These include the following:
- Overactive thyroid
- Disorders of the adrenal glands
- Overactive parathyroid glands
- Disorders of the pituitary gland
Of course, non-hormone related issues may also increase the risk of developing osteoporosis, including:
- Family history of this disease
- Low BMI (19 or less)
- Having an eating disorder
- Heavy drinking or smoking
- Arthritis
- Long-term periods of inactivity like bed rest
Symptoms of osteoporosis
As mentioned before, osteoporosis can be a silent disease. This means it does not present any sure symptoms and you would not be able to feel your bones growing weaker. Therefore, osteoporosis is mostly undetected until you suddenly break a bone.
There are some things you can look for which could indicate bone weakness. If you notice these, you may want to chat with your doctor to get to the cause of the issue:
- Severe back pain
- Curving of the spine, especially with older age
- Unexpected weight loss
Osteoporosis prevention
Your genes are indeed responsible for your height and the strength of your skeleton, however, several lifestyle factors such as diet and exercise are also critical in their influence on your bone health.
Here are some things you can do to keep your bones healthy (World Osteoporosis day, 2021):
- Exercise regularly
For adults aged 19-64 regular exercise is essential and it is recommended that they do at least 2.5 hours of moderate-intensity activity weekly. This includes fast walking, jogging, or cycling.
Weight-bearing exercise and resistance exercises are even more important for improving bone density and preventing osteoporosis. Adults should do muscle-strengthening exercises 2 or more days per week by working all major muscle groups – legs, arms, hips, back, abs, chest, and shoulders.
Exercises such as running, skipping, dance, aerobics are all very useful for strengthening muscles, ligaments and joints. People who are older than 60 can also benefit from these exercises at their own pace.
- A healthy diet and Vitamin D
Eating healthy is recommended for everyone. It can help prevent various health conditions including heart disease, diabetes, and many forms of cancer. This also includes reducing the risk of developing osteoporosis.
Calcium is vital for strong bones. It is recommended that adults consume 700mg a day through food such as milk, cheese, leafy green vegetables like kale, dried fruit, tofu, and fish where you eat the bones (e.g., sardines).
Vitamin D is also fantastic for healthy bones and teeth as it helps with calcium absorption. The recommended daily amount for adults is 10micrograms and good sources include oily fish, red meat, egg yolks and fortified foods like some fat spreads or breakfast cereals.
Additionally, from late March/early April to the end of September sunlight will be great for you as it triggers the production of vitamin D (NHS, 2020).
- Drink less and quit smoking
Both smoking and misuse of alcohol are associated with an increased risk of osteoporosis. Don’t drink more than the recommended 14 units of alcohol per week and avoid binge drinking.
Quitting smoking will not only reduce the risk of developing osteoporosis but also other diseases associated with the lungs such as lung cancer or bronchitis.
- Regular testing
Some recommend attending regular screenings from age 40-50 depending on your risk group or if you have a family history.
There are several treatments that people who are diagnosed with osteoporosis can go through to prevent, reduce and/or manage their condition. Only through regular tests, you will be able to catch changes in your bones and get ahead of the issue.
Best scan for diagnosing Osteoporosis
The most common way of detecting osteoporosis is through a bone density scan. A CT bone density scan is accurate in measuring the density of your bones and determining the presence of osteoporosis and the risk of future bone fracture in your hips or spine (National Osteoporosis Foundation, 2021).
Many public healthcare providers use the DEXA scan to assess bone density, but CT bone density scans are better as they are the only means of measuring the real volume density of the middle of the vertebrae. A CT bone scan provides measurements of volume density (mg/cm3) of the spine and is not subject to being affected by external influences like lymph nodes.
A study conducted in 2013 found that osteoporosis was diagnosed only in 17.1% of the 140 participants using a DEXA scan, compared to 46.4% using the CT bone density scan (Li et al., 2013). This is because the CT scan is more sensitive and can detect osteoporosis better.
Another study from 2005 demonstrated that the DEXA scan cannot account for the large variability in skeletal size and composition in growing children (Wren et al., 2005). While osteoporosis is not extremely common among younger people or kids, it is clear that CT scans are better adapted to detect this disease for people of any age.
Detection of osteoporosis at an early stage offers the chance for effective treatment to be applied, which can slow or even reverse the loss of bone density and reduce future risks.
Head to toe assessment at Echelon Health
The team at Echelon Health believes that prevention is key for a healthy long life, and we are proud to offer a range of health screenings for the diseases which may be growing inside your body without showing any symptoms.
Our Platinum Assessment uses state of the art advanced imaging technology and scans to detect up to 94% of the conditions that contribute to premature death among males and females.
Echelon Health’s comprehensive Platinum Assessment in London will include scans for the following diseases for your full peace of mind:
- Vascular Dementia
- Cerebrovascular Disease
- Arteriovenous Malformation
- Brain Cancer
- Cancer of Sinuses
- Acoustic Neuroma
- Carotid Artery Atheroma
- Thyroid Cancer
- Lung Cancer
- Acute Lung Diseases
- Aortic Aneurysm
- Chronic Respiratory Disease
- Pulmonary Fibrosis
- Coronary Heart Disease
- Breast Cancer
- Skin Cancer
- Liver Cancer
- Spleen Enlargement
- Gallbladder Disease
- Adrenal Gland Tumours
- Kidney Cancer
- Diverticular Disease
- Colorectal Cancer
- Bladder Cancer
- Prostate Cancer
- Testicular Cancer
- Cancer of the Ovaries
- Osteoporosis
To learn about the scans, we use to detect these diseases, check out our Body Map which easily explains what each scan is used for and why.
Our world-class team of radiologists and doctors make use of the most advanced medical imaging technology available, meaning you are in the best hands.
Sources:
World Osteoporosis day (2021). About osteoporosis. Available at: https://www.worldosteoporosisday.org/about-osteoporosis (Accessed 20/10/2021).
Age UK (2021). Osteoporosis. Available at: https://www.ageuk.org.uk/information-advice/health-wellbeing/conditions-illnesses/osteoporosis/ (Accessed 20/10/2021).
NHS (2019). Causes Osteoporosis. Available from: https://www.nhs.uk/conditions/osteoporosis/causes/ (Accessed 20/10/2021).
Wren, T. A., Liu, X., Pitukcheewanont, P., & Gilsanz, V. (2005). Bone densitometry in pediatric populations: discrepancies in the diagnosis of osteoporosis by DXA and CT. The Journal of pediatrics, 146(6), 776-779.
Li, N., Li, X. M., Xu, L., Sun, W. J., Cheng, X. G., & Tian, W. (2013). Comparison of QCT and DXA: osteoporosis detection rates in postmenopausal women. International Journal of Endocrinology, 2013.
NHS (2020). Overview: Vitamins and minerals. Available at: https://www.nhs.uk/conditions/vitamins-and-minerals/ (Accessed 20/10/2021).
National Osteoporosis Foundation (2021). Bone Density Exam/Testing. Available at: https://www.nof.org/patients/diagnosis-information/bone-density-examtesting/ (Accessed 20/10/2021).